When it comes to understanding and diagnosing heart health, there’s a myriad of tests and examinations that medical professionals rely on. Among these, blood tests play a crucial role in providing insights into the state of our cardiovascular system. But the question often arises: Can a blood test detect a heart issue? In this blog post, we’ll delve into the capabilities of blood tests in detecting heart issues, the specific types of tests available, and what these tests can tell us about our heart health.
Understanding Heart Issues
Heart issues can range from minor abnormalities that require monitoring to critical conditions that necessitate immediate intervention. Heart attacks, arrhythmias, heart failure, and coronary artery disease are a few of these ailments. Symptoms might be as subtle as fatigue or as severe as chest pain and shortness of breath. Given the heart’s vital role in pumping blood throughout the body, detecting and addressing these issues early can be life-saving.

The Role of Blood Tests in Diagnosing Heart Issues
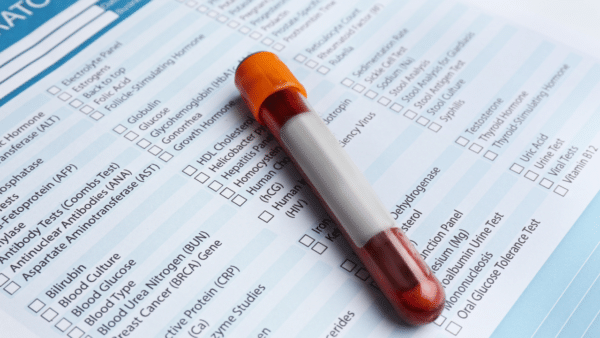
Blood tests are a window into the body’s inner workings, offering clues that can help diagnose a range of conditions, including those affecting the heart. While a blood test alone cannot provide a complete picture of heart health or diagnose all heart conditions, it can offer critical information that, when combined with other tests and a clinical examination, contributes significantly to understanding a patient’s cardiovascular health.
Types of Blood Tests for Heart Health
Several blood tests are specifically used to detect issues related to the heart:
- Lipid Profile: The lipid test quantifies the blood’s concentrations of various triglycerides and cholesterol. Elevations in triglycerides and low-density lipoprotein (LDL), commonly referred to as “bad” cholesterol, have been linked to a higher risk of coronary artery disease.
- High-Sensitivity C-Reactive Protein (hs-CRP): Elevated levels of hs-CRP can indicate inflammation in the body, which is a risk factor for heart disease.
- Natriuretic Peptides (BNP and NT-proBNP): These tests measure the levels of B-type natriuretic peptide and its precursor. High levels can indicate heart failure, as these peptides are released by the heart when it’s under stress or functioning abnormally.
- Cardiac Enzymes (Troponin T and I): These proteins are released into the bloodstream when the heart muscle is damaged, such as during a heart attack. Elevated troponin levels are a key indicator of myocardial infarction.
- Homocysteine: Elevations of the blood amino acid homocysteine have been associated with a higher risk of stroke and coronary artery disease.
What Can Blood Tests Tell Us?
Blood tests can provide valuable information about risk factors for heart disease. For example, a lipid profile can alert doctors and patients to the need for lifestyle changes or medication to manage cholesterol levels. Similarly, elevated hs-CRP levels can prompt further investigation into potential sources of inflammation and cardiovascular risk.
In acute situations, such as when a heart attack is suspected, measuring cardiac enzymes like troponin is crucial for diagnosis and guiding treatment. The presence of these enzymes in the blood can confirm that heart damage has occurred, allowing for timely and appropriate medical intervention.
Signs and Symptoms of Heart Issues
Recognizing the signs and symptoms of heart issues is crucial for early detection and treatment. While some heart conditions may be silent or only show mild symptoms, others present clear warning signs. Here are some common symptoms that could indicate a heart problem:
- Chest Pain or Discomfort: Often described as a feeling of pressure, squeezing, fullness, or pain in the center or left side of the chest, which may last for a few minutes or come and go.
- Shortness of Breath: Difficulty breathing or feeling winded at rest or during physical activity.
- Fatigue: Unusual tiredness can be a symptom, especially if it’s more pronounced during times of rest or with minimal exertion.
- Palpitations: Irregular heartbeats that feel like a fluttering or racing heart.
- Swelling: Edema, or swelling in the ankles, legs, feet, or abdomen, can be a sign of heart failure, where the heart is unable to pump blood effectively.
- Dizziness, Lightheadedness, or Fainting: These symptoms can occur if the heart is not pumping enough blood to the brain.
Not every cardiac condition has obvious warning indicators. Not every frightening chest grip is accompanied with a floor fall, unlike what you may see in movies. There are cardiac symptoms that do not even occur in the chest, and diagnosing them is not always simple. It is critical to get medical help right away if you think you or someone else is having a heart attack.

Who Suffers From Heart Issues Statistically
Millions of individuals across diverse demographics are impacted by heart disease, which continues to be one of the world’s top causes of mortality. But some groups are more vulnerable than others, and identifying these tendencies can improve the effectiveness of prevention and treatment programs.
- Age: The risk of heart disease increases with age for both men and women. People aged 65 and older are more likely to suffer from heart disease compared to younger individuals.
- Gender: Historically, men have been at a higher risk of heart disease at an earlier age. However, after menopause, the risk for women increases and can surpass that of men.
- Ethnicity: Certain ethnic groups have a higher predisposition to heart disease. For example, in the United States, African Americans are more likely to have heart disease than Caucasians, partly due to higher rates of hypertension, obesity, and diabetes in this group.
- Family History: Genetics play a significant role. Having a close relative who has had heart disease increases your risk, especially if the relative was a parent or sibling and was diagnosed at a younger age.
- Lifestyle Factors: Poor diet, smoking, lack of exercise, and excessive alcohol use can significantly increase the risk of developing heart disease, regardless of your background.
It is critical to comprehend these figures, but it is equally critical to keep in mind that anyone might have heart disease. Prevention and early identification can be significantly aided by alterations in lifestyle, routine examinations, and awareness of the symptoms.
Beyond Blood Tests
While blood tests are invaluable, it’s important to remember they are part of a larger diagnostic toolkit. Other tests, such as electrocardiograms (ECGs), echocardiograms, stress tests, and coronary angiograms, are also essential in diagnosing heart conditions. A comprehensive evaluation by a healthcare provider, considering both blood test results and other diagnostic information, is necessary to accurately assess heart health.
Conclusion
In summary, blood tests are an important tool for diagnosing cardiac problems. They can direct additional testing and treatment by offering early alerts of risk factors and acute diseases. They are only one component of the diagnostic puzzle for heart disease, though. It is critical to speak with a healthcare professional if you or someone you love is worried about their heart health. They can suggest the right tests and interpret the findings in light of your overall health.
Remember, heart health is influenced by a combination of factors, including genetics, lifestyle, and environmental factors. Regular check-ups, a healthy diet, regular physical activity, and monitoring your health through tests recommended by your healthcare provider can all contribute to a healthier heart and a longer, more vibrant life.